by Bryn Nelson, PhD
Opportunities to be more efficient are largely under care of hospitalists, ACO director says
 Several years ago, Presbyterian Medical Group in Albuquerque, N.M., decided to integrate three elements of its healthcare system: its health plan, the employed medical group, and the hospital delivery system. Knitting those parts into a cohesive whole helped the group realize that “lowering the cost of care by improving efficiency, by improving coordination, and by enhancing collaboration between payor and physicians made a lot of sense,” executive medical director David Arredondo, MD, says. When the accountable care organization (ACO) concept came along, Dr. Arredondo says, “it really was just a natural extension of what we were doing.”
Several years ago, Presbyterian Medical Group in Albuquerque, N.M., decided to integrate three elements of its healthcare system: its health plan, the employed medical group, and the hospital delivery system. Knitting those parts into a cohesive whole helped the group realize that “lowering the cost of care by improving efficiency, by improving coordination, and by enhancing collaboration between payor and physicians made a lot of sense,” executive medical director David Arredondo, MD, says. When the accountable care organization (ACO) concept came along, Dr. Arredondo says, “it really was just a natural extension of what we were doing.”
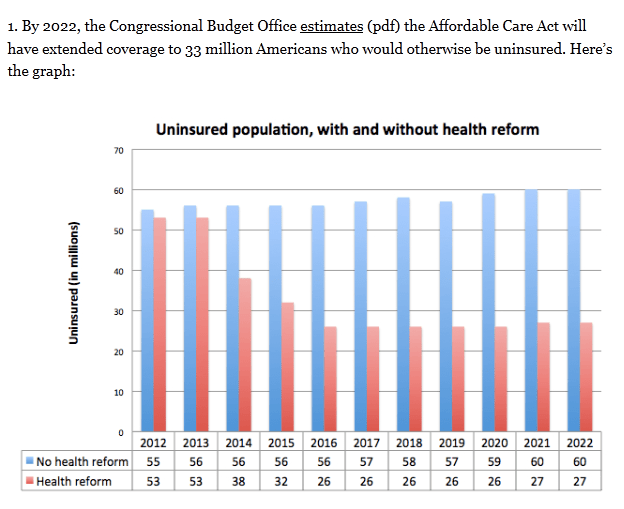
The ACO model, championed as a way to prevent the fragmentation of care and rein in costs by getting providers to assume joint responsibility for specific patient populations, received a major boost through 2010’s Affordable Care Act. Last year’s ACO rule-making process by the Centers for Medicare & Medicaid Services (CMS), however, was anything but smooth. Cautious optimism by such organizations as SHM gave way to loud complaints over the initial rules for a voluntary initiative called the Shared Savings Program. Critics asserted that participants would be forced to assume too much financial risk while being swamped with paperwork requirements.
By year’s end, though, the final rules had assuaged many of the biggest concerns, and the April 10 announcement of 27 participants for the program’s first round—more than half of which are physician-led organizations—has rekindled much of the enthusiasm. According to CMS officials, the agency is reviewing more than 150 applications for the program’s next round, which will begin in July.
Keys to Success
In December, CMS selected 32 organizations to participate in an even more ambitious initiative called the Pioneer ACO Model. That separate but related experiment in shared accountability launched Jan. 1, and it may be months before enrolled organizations can say whether the rewards outweigh the risks. Interviews with Presbyterian’s Dr. Arredondo and two other Pioneer participants about why they took the plunge, however, have highlighted some potential keys to success.
All three agree that the ACO model offers a better match for their long-term, patient-centered goals and that the fee-for-service model is gradually becoming a thing of the past.
“In some ways, it was actually kind of a relief that the system was going this way because we, probably like many systems, were beginning to be caught between the budgeted model and a fee-for-service model,” Dr. Arredondo says. “When you’re heavily one way or heavily the other way, then it makes things a little easier to manage and understand. When you’re right in the middle, it becomes a little uncomfortable.”
Penny Wheeler, MD, chief clinical officer for Minneapolis-based Allina Hospitals & Clinics, says organizations in that precarious position need to carefully examine their capabilities and consider how best to pace their transition. Otherwise, they might prematurely give up too much revenue that could be used to reinvest in care improvements.
“We can tolerate it if we shoot ourselves in one foot, but we can’t tolerate it if we shoot ourselves in both feet, in this new world,” Dr. Wheeler says.
If caution is warranted, she says, the ACO model still aligns well with a strategy of building toward outcome-based healthcare. Despite the likelihood of “lumps and bumps and warts along the way,” Dr. Wheeler says, “we really wanted to be part of the shaping of that outcome-based delivery, and receive market rewards for what we were creating for our community.”
Austin, Texas-based Seton Health Alliance, a third Pioneer participant, is a collaborative effort between a hospital delivery system known as Seton Health Care Family and a multispecialty physician group called Austin Regional Clinic. Greg Sheff, MD, president and chief medical officer of the ACO, says the partnering organizations were separately moving toward more population health initiatives and more proactive, coordinated, and accountable care.
“The Pioneer ACO, for us, really provided an opportunity to light the fire and motivate the organizations to put the entity together and start doing the work,” he says, adding PCPs and hospitalists will be critical to his organization’s ongoing integration efforts.
“The areas where there are opportunities to be more efficient are largely under the care of the hospitalists,” he says, citing in-house utilization as well as care transitions, comprehensive post-acute placement, and readmission prevention efforts. To support those providers, Pioneer participants say well-designed electronic medical records are paramount, while separate efforts, such as patient-centered medical homes and unit-based rounding, might offer timely assists. (Click here to listen to more of The Hospitalist’s interview with Dr. Sheff.)
No one’s expecting the next few years to be seamless, but Dr. Sheff views his newly formed ACO as a long-term endeavor in which success isn’t necessarily defined by whether the group achieves shared cost savings.
“We define success by whether we are able to move our delivery system to a place where we’ll be much more adept at going forward, continuing to manage populations,” he says. “We really see this as a strategic organizational decision more than, ‘Boy, that contract looks like something that we can leverage in the short term.’”
Bryn Nelson is a freelance medical writer in Seattle.
This article originally appeared in The Hospitalist.