by Gregg Anthony Masters, MPH Some of you may have heard about the whining by UnitedHealthcare’s leadership on a recent earnings call which included the required ‘management’s discussion or operating results and market conditions’ analysis. A BIG WHAAAA! Overfunded since inception and having perfected the art of ‘upcoding‘ (i.e,, severity of illness and intensity of …
Tag Archives: health reform
ACO Digital Assets Available
by Gregg A. Masters, MPH It’s been quite some time that I’ve updated this site though not for a lack of news. Yet some 434 posts later following the rollout of the Affordable Care Act, the signature, and against all odds accomplishment of then President Barack Obama, I thought I’d update both subscribers and followers …
Need Another Acronym? Think ‘CHART’ Courtesy of ‘CMMI’
by Gregg A. Masters, MPH In a sea of relentless ‘acronym soup’ that peppers the landscape and too often separates us from the constituency we ostensibly serve (patients) via added layers of dubious complexity to the dysfunctional U.S. healthcare delivery and financing ecosystem, the Centers for Medicare and Medicaid Innovation (CMMI) has added the ‘Community …
Continue reading “Need Another Acronym? Think ‘CHART’ Courtesy of ‘CMMI’”
National Association of ACOs et al Weigh in on the ‘Value in Health Care Act of 2020’
by Gregg A. Masters, MPH Article discovered via the National Association of ACOs (NAACOs) a ‘501 (c) 6 non-profit organization that allows Accountable Care Organizations (ACOs) to work together to increase quality of care, lower costs and improve the health of their communities’ . NAACOs et al weigh in on the Value in Health Care …
Health Care ‘Texas Style’: A Model for the Nation?
By Gregg A. Masters, MPH This a re-post of an article written in October 2009 following Atul Gawande‘s article in the New Yorker on the ‘cost conundrum‘ which launched his presence and eventual celebrity on the national stage. Gawande was calling attention to the regional variations (small area analysis) in the Medicare spend and associated …
Continue reading “Health Care ‘Texas Style’: A Model for the Nation?”
ACOs and Value Based Care: The Best of Times Or The Worst of Times? It Depends!
By Fred Goldstein, MS and Gregg Masters, MPH This past year has seen major changes to the Medicare Shared Savings Program (MSSP) that launched the huge growth in Accountable Care Organizations (ACOs) a principal workhorse in the transformational copy of the Affordable Care Act (ACA). It seems that the Center for Medicare and Medicaid Services …
Continue reading “ACOs and Value Based Care: The Best of Times Or The Worst of Times? It Depends!”
U.S. Department of Health and Human Services Office of Inspector General: ACOs’ Strategies for Transitioning to Value-Based Care – Lessons From the Medicare Shared Savings Program
by Gregg A. Masters, MPH Many have suggested ACOs would not make a dent in restraining the growth of the U.S. healthcare spend, nor have a meaningful impact on elevating the quality of care provided to covered members or beneficiaries (patients). From ‘HMO-lite‘ criticism to a range of ‘tepid’ to no patient channeling mechanisms, recent …
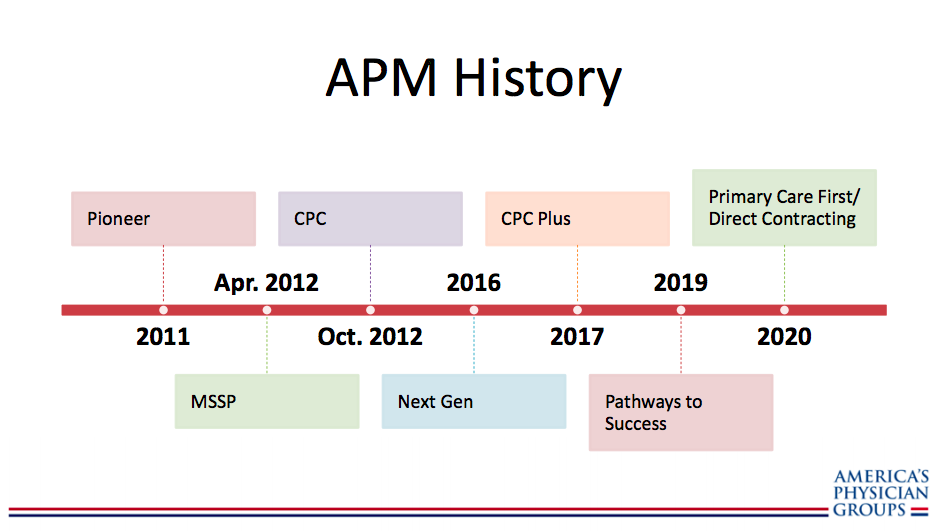
APG: Overview of CMMI New Models – Primary Care First and Direct Contracting
by Gregg A. Masters, MPH The future is already here, it’s just unevenly distributed – Attributed to William Gibson As a soldier mainstreaming both HMOs and (‘attorney in fact‘ vs. messenger model) 2nd generation PPOs (that re-priced claims to contract rates) into ‘mainstream medicine‘ in California vs. the then prevailing 2nd or 3rd tier physician/provider …
Continue reading “APG: Overview of CMMI New Models – Primary Care First and Direct Contracting”
Venrock’s 2019 Healthcare Prognosis
by Gregg A. Masters, MPH Received this embargoed report earlier this week. Venrock has formally released the report this morning. One reason I am fond of their work is I’ve been following Bob Kocher, one of Venrock’s principals, since the turbulent introduction of the ACA by the Obama administration. More recently perhaps due to Venrock’s …
On Lessons NOT Learned from Managed Healthcare v1.0 and Beyond
by Gregg A. Masters, MPH First in a series of lessons NOT learned tweets to be enhanced and re-posted to @ACOwatch. In the 80s Sanford C. Bernstein analyst Kenneth Abramowitz predicted for-profit hospital systems would dominate the market by 2000. One of the strategy ‘diversification arrows‘ in the quiver of hospital system executives was to enter the …
Continue reading “On Lessons NOT Learned from Managed Healthcare v1.0 and Beyond”