By Gregg Anthony Masters, MPH
January 13, 2026
Here’s the thing.
Healthcare leadership is rarely bold and too often ‘MIA’ when it comes the hard (risky) work of transforming our dysfunctional by design healthcare delivery and financing model about to implode on itself.
They’re generally risk averse and lazy bunch, preferring the hedge of ‘me too’ (what are my colleagues implementing?) strategies vs. the vision (and risk) of innovation’s upside potential when it comes to the transformational imperative to enable the triple aim (better care, superior outcomes at a lower per capita spend).
I’ve been in the ‘innovation space’ since the 80s in Southern California teaching doctors and hospital executives on the potential upside of managed care particularly as the model morphed away from closed loop systems (staff and group models) into a better fit with mainstream medicine, i.e, the IPA (Independent Practice Association).
Back in the day, HMOs were relegated to these limited and closed networks that primarily attracted 2nd and 3rd tier docs, often FMGs (foreign trained medical graduates) and the cohort within medicine that preferred the security of a salary at a staff or group model HMO vs. the entrepreneurial impulse to build a practice.
Amid current efforts to destroy vs. improve the ACA (Affordable Care Act) by defunding premium subsidies, here’s what we refuse to face, or that nobody wants to say out loud from the podium on social media, at networking parties or Congressional hearings:
With the advent of Maxicare’s ‘Window Project’ the penetration of mainstream medicine went full throttle to integrate HMOs into the growing pool of employer sponsored group health benefit plans, often side by side with ‘vote with your feet’ PPOs’. While also giving birth to the MSO (Management Services Organization) industry that provided essential infrastructure to assume and thrive under coordinated capitated payment terms.
The Lie We Keep Telling Ourselves
‘Medicare Advantage’ (MA) is NOT Medicare!
Let me translate: UnitedHealth coded harder, faster, and more aggressively than anyone else and got paid billions more because of it.
It’s not just a semantic quibble, nor splitting hairs per se. And it’s sure as hell not the technicality the MA lobby wants you to think it is.
Medicare Advantage is a term-limited contract with a private operator (MA plan) under Part C where CMS (the Centers for Medicare and Medicaid Services) ‘assigns’ the per member per year (PMPY) funds to the operator to administer Medicare-covered benefits under a capitation system. These terms and associated benefits are for one year. The operator can exit or change the contract terms, networks, formularies, utilization controls, and cost-sharing every single year. That’s not Medicare. That’s a commercial product wearing Medicare’s name tag.
As of January 12, 2026, the United States Senate just shoved that uncomfortable truth back into the national spotlight with a 105-page evisceration of UnitedHealth Group’s Medicare Advantage playbook.
Grassley Drops the Hammer: UnitedHealth and the Industrialization of ‘Diagnosis Capture’
Senator Chuck Grassley (R-Iowa), Chair of the Senate Judiciary Committee, released a majority staff report today that reads less like oversight and more like a forensic audit of a company that turned Medicare Advantage risk adjustment into its own profit-generating machine.
The thesis? UnitedHealth Group, the $400+ billion healthcare ‘too big to sail’ colossus that owns UnitedHealthcare, Optum, and effectively controls 10 million+ MA lives, has weaponized “diagnosis capture” including severity of illness/intensity of service upcoding at industrial scale.
According to the report, the MA scheme machinery includes:
- In-home health risk assessments (HRAs) conducted by nurse practitioners whose job it is to find billable diagnoses
- Secondary chart reviews by professional coders hunting for missed revenue opportunities
- Pay-for-coding incentives to external clinicians – literally paying doctors to document more
- Vertically integrated providers whose EHR workflows can be shaped by the parent company
- AI-powered analytics identifying diagnosis opportunities where clinical thresholds are “squishy” (their word, not mine)
This isn’t a one-off compliance issue. This is the systemic architecture of a ‘healthcare borg’ that assimilates all material innovations intent on the transforming our paradigm from a fee-for-services, ‘do more to earn more’ model to one focused on the right patient, right care, right setting and time alchemy of a medical necessity driven model.
Grassley’s staff reviewed 50,000 pages of UnitedHealth documents including training materials, internal policies, software tools, audit protocols, etc., and concluded that UnitedHealth “turned risk adjustment into a major profit-centered strategy, which was not the original intent of the program.”
Industry publication Healthcare Dive reports that UnitedHealth “strategically captured a higher number of diagnoses and diagnosis codes than any other MA insurers – also resulting in higher CMS reimbursement than any of its peers.”
Now, UnitedHealth disputes the framing. They say their programs comply with CMS requirements and audits. Fine. But here’s the policy question that transcends any single actor:
Can a public program remain financially and clinically coherent when private plans are paid based on diagnoses, they are financially motivated to find?
OIG Already Told Us This – With Receipts!
If you want to know whether “diagnosis capture” is real, don’t read corporate press releases. Read watchdogs, including ACO Watch.
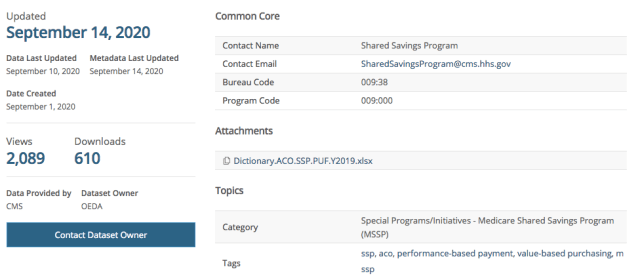
In October 2024, the HHS Office of Inspector General reported that diagnoses submitted only on HRAs and HRA-linked chart reviews, with no other service records tied to those diagnoses, drove an estimated $7.5 billion in MA risk-adjusted payments for 2023.
Read that again: Diagnoses that didn’t show up anywhere else in the encounter data still drove billions in payments.
STAT News’ coverage noted that UnitedHealth alone accounted for $3.7 billion of that $7.5 billion, almost half the total.
OIG’s point wasn’t “HRAs are always bad.” It was more damning: HRAs are vulnerable to misuse because they’re frequently administered by plans or vendors rather than a patient’s own treating clinicians.
The lack of any other follow-up visits, procedures, tests, or supplies for 1.7 million MA enrollees raises concerns that either:
- The diagnoses are inaccurate (and thus the payments are improper), or
- Enrollees didn’t receive needed care for serious conditions
Either way, taxpayers once again are the ‘bag holders’ for corporate greed..
MedPAC has been ringing the same alarm bells for years: MA risk scores remain higher than they would have been in traditional Medicare even after statutory adjustments, and coding intensity varies wildly across plans.
GAO documented years ago that coding differences can inflate risk scores and drive excess payments beyond what CMS adjustments have historically offset.
So, when a Senate report alleges a major payer optimized that vulnerability with uncommon scale and sophistication, it lands on pre-softened ground.
The Nursing Home Story: When Capitation Conflicts with Clinical Judgment
While Grassley’s report focuses on payment coding mechanics, there’s a second Senate track that’s even darker.
Senate Finance Committee leaders Ron Wyden (D-Ore.) and Elizabeth Warren (D-Mass.) have been investigating allegations related to UHG/Optum programs in nursing homes, specifically whether incentive structures designed to reduce hospital transfers create dangerous conflicts of interest.
A January 8, 2026 follow-up letter presses UHG for documents and details, citing heightened concerns and reported adverse outcomes, including at least three nursing home residents who allegedly died after being denied hospital transfers.
STAT reports that The Guardian’s December 2025 investigation spotlighted allegations that UnitedHealth’s cost-reduction programs may have resulted in deaths.
If the coding story is about who gets paid and why, the nursing home story is about something even more visceral:
What happens when the entity holding the capitation also influences whether a frail elder gets transferred to the hospital?
In managed care, “reducing unnecessary hospitalizations” can be good medicine. It can also be cost containment dressed up as care transformation. The line isn’t always bright which is exactly why Senate oversight matters here.
The Brand Problem: Stop Calling It “Medicare”
Now let’s talk about the part nobody wants to say out loud because it sounds too obvious:
If MA were truly “Medicare,” it wouldn’t need to borrow Medicare’s name to sell itself.
CMS has tightened marketing oversight in recent years, including rules addressing misleading impressions and third-party marketing behavior. The 2023 final rule explicitly prohibits using the Medicare name or logo in a “misleading way.”
Yet the market reality remains: Consumers experience a daily blur of ads that imply they are “upgrading Medicare” rather than switching into a private plan with rules, restrictions, and networks.
So, here’s my position, plainly:
· MA is a private contract (Part C), not the Medicare program (Parts A & B under statute).
· Advertising should never use “Medicare” as a branding shortcut that obscures the private nature of the coverage.
· At minimum, any marketing that uses “Medicare” prominently should be required to state prominently, that it is a non-government plan option and not the Medicare program itself.
This is not anti-choice. It’s pro-informed consent.
The Selection Problem: Cherry-Picking Without the Cherry-Picking
MA plans are required to accept all applicants in their service area during appropriate enrollment periods, but “selection” doesn’t only happen through formal denial.
It happens through:
- Network design
- Benefit design
- Marketing segmentation
- Broker incentives
- Friction (or ease) in switching
The evidence base supports concern about favorable selection into MA even after risk adjustment.
KFF’s analysis notes that people who enroll in MA spent $1,253 less per year in traditional Medicare before they switched, even after risk adjustment. That’s not MA making them healthier. That’s MA attracting healthier people. Let that sink in!
Research published in Health Affairs found that favorable selection into MA led to an average of $9.3 billion per year in overpayments between 2017 and 2020.
KFF has also documented that people who disenroll from MA tend to have higher spending than similar beneficiaries who remain in traditional Medicare, consistent with risk dynamics and churn that can disadvantage higher-need individuals.
The Urban Institute’s comprehensive review concludes: “consistent and convincing evidence shows that favorable selection, after accounting for risk adjustment, is a key contributor to MA overpayment.“
When you combine favorable selection with coding intensity, you get a plausible recipe for a program that looks efficient while shifting financial pressure back onto the statutory Medicare program and taxpayers.
The Counterargument: MA Delivers ‘Value’ – Sometimes Real, Sometimes Theater
If we’re going to be credible, we must acknowledge what MA does offer:
- An out-of-pocket maximum for Part A/B services (traditional Medicare does not have one unless paired with Medigap or other supplemental coverage)
- Supplemental benefits (dental/vision/hearing and more) that many beneficiaries want and use
- In many markets, lower premiumsand“bundle convenience,” including formulary (PBM) driven integration of Part D (the prescription drug plan)
Industry advocates also argue that some widely cited “overpayment” estimates are inflated by methodology and ignore program differences (like supplemental benefits and OOP – out of pocket- limits).
That’s the debate. But here’s the pivot:
Even if MA can deliver consumer value, it does not follow that “coding games” and “misleading branding” are acceptable collateral damage.
We can preserve consumer-facing benefits AND reform the incentives that distort coding, care, and communication.
What Reform Could Look Like (Without Blowing Up Choice)
Here’s a practical reform stack—built from watchdog findings and policy logic, not ideology:
1. Stop Paying for “HRA-Only” Diagnoses Without Corroboration
OIG’s findings make this the low-hanging fruit: If a diagnosis exists only in a plan-driven assessment and never appears in follow-up care or encounter records, it should not drive payment without additional evidence.
2. Strengthen RADV and Data Validation with Real Consequences
The MA payment engine runs on diagnosis data. Audits have to be scalable, timely, and consequential, or they become theater.
3. Align Risk Adjustment with Clinical Action, Not Just Documentation
If diagnosis capture is “real,” it should show up as care plans, monitoring, meds, referrals, or resource use. If it doesn’t, why is Medicare paying as if it does?
4. Truth-in-Advertising: Stop Calling MA “Medicare”
Make the distinction unavoidable in marketing:
- “a Private plan option“
- “Not the Medicare program”
- “Plan networks and prior authorization may apply”
- Plain-English trade-offs
5. Rebalance Incentives So Plans Win by Keeping People Well, Not by Finding Codes
Risk adjustment is necessary, but it shouldn’t be a profit center.
Bottom Line: The Medicare Brand Must Mean Something
The Senate’s scrutiny of UnitedHealthcare, paired with watchdog evidence on coding intensity, should be a wake-up call for policymakers, providers, and patients.
This is not a niche compliance squabble. It’s a structural integrity issue for a massive public-private hybrid that now covers tens of millions of older adults, including this author.
If you want to keep Medicare sustainable, you need two kinds of honesty:
- Payment honesty (diagnoses should reflect reality and care), and
- Marketing honesty (Medicare Advantage is not Medicare)
Because when a private contract markets itself as a public promise, and when diagnosis codes become a revenue stream, we don’t just risk overpayment.
We risk public trust.
And once that’s gone, good luck sailing anything – Medicare included.
==##==
** AI provided an assist via background research, organization and validation of claims as supported or challenged by authoritative 3rd parties, ie, academia, government, NGO or industry sponsored case studies.
Quick FAQ
Is Medicare Advantage the same as Medicare?
No. Medicare Advantage (Part C) is offered by private insurers under contract with CMS; Original Medicare is the federal program (Parts A & B).
Why is MA under Senate scrutiny?
Senate investigators are examining whether some MA practices—such as aggressive diagnosis capture for risk adjustment—may inflate payments, and whether certain care models create problematic incentives (e.g., nursing home hospital transfer decisions).
What is “risk adjustment” in MA?
CMS pays plans more for members coded as sicker (higher risk scores) to discourage avoiding high-need patients—yet it creates incentives to maximize diagnoses.
Do MA plans have benefits Original Medicare doesn’t?
Often yes—out-of-pocket limits for Part A/B services and supplemental benefits like dental/vision/hearing are common.
Source Documents & Further Reading
Senate Reports
OIG Reports & Investigations
MedPAC Analysis
GAO Reports
CMS Marketing Rules & Regulations
KFF Research & Analysis
Urban Institute Research
Additional Analysis & Coverage
Gregg Masters, MPH, is a health policy analyst, public health and patient safety advocate and founder of ACOWatch.me. Follow him on social media @GreggMastersMPH or visit www.EndNMP.org or 2healthguru.wordpress.com for more analysis.








 :
:
