by Gregg Anthony Masters, MPH Some of you may have heard about the whining by UnitedHealthcare’s leadership on a recent earnings call which included the required ‘management’s discussion or operating results and market conditions’ analysis. A BIG WHAAAA! Overfunded since inception and having perfected the art of ‘upcoding‘ (i.e,, severity of illness and intensity of …
Tag Archives: cms
Need Another Acronym? Think ‘CHART’ Courtesy of ‘CMMI’
by Gregg A. Masters, MPH In a sea of relentless ‘acronym soup’ that peppers the landscape and too often separates us from the constituency we ostensibly serve (patients) via added layers of dubious complexity to the dysfunctional U.S. healthcare delivery and financing ecosystem, the Centers for Medicare and Medicaid Innovation (CMMI) has added the ‘Community …
Continue reading “Need Another Acronym? Think ‘CHART’ Courtesy of ‘CMMI’”
ACOs and Value Based Care: The Best of Times Or The Worst of Times? It Depends!
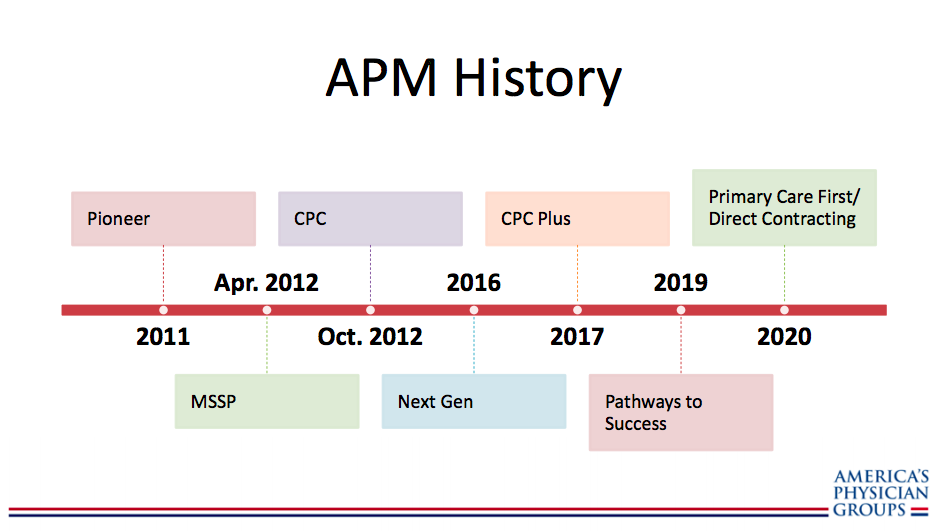
By Fred Goldstein, MS and Gregg Masters, MPH This past year has seen major changes to the Medicare Shared Savings Program (MSSP) that launched the huge growth in Accountable Care Organizations (ACOs) a principal workhorse in the transformational copy of the Affordable Care Act (ACA). It seems that the Center for Medicare and Medicaid Services …
Continue reading “ACOs and Value Based Care: The Best of Times Or The Worst of Times? It Depends!”
Founder and CEO of ACO Management Company Weighs in on Regulatory Uncertainty
by Gregg A. Masters, MPH It’s been a while since my last post. I hope everyone is enjoying their summer. In California we’re dealing with very serious wildfire threat. Please hold space in your thoughts and prayers for all of those in harms way – especially the first responders putting their lives on the line …
Continue reading “Founder and CEO of ACO Management Company Weighs in on Regulatory Uncertainty”
Center for Medicare and Medicaid Services Releases Accountable Care Organization Performance Results
by Gregg A. Masters, MPH Friday, October 27th, the Center for Medicare and Medicaid Services (CMS) released details for participating Accountable Care Organizations (ACOs) in the Medicare Shared Savings Program (MSSP) for the 2016 performance year. For reporting ACO results view the entire report here. The National Association of ACOs (NAACOs) weighed in below: The new results …
ACOs Fudging the Numbers?
by Gregg A. Masters, MPH I came across this piece on the Healthcare Blog penned by Kip Sullivan, Esq, critiquing this article posted in Health Affairs last May ‘Bending The Spending Curve By Altering Care Delivery Patterns: The Role Of Care Management Within A Pioneer ACO‘. Sullivan raises valid points as the the legitimacy of …
Webinar: Next Generation ACO Model – Overview and LOI Information
By Gregg A. Masters, MPH Today marks the end to the eight year reign of President Barack Obama and the birth of the Trump Administration tenure. Yet, so much in the health policy and reform domain remains unclear and on the come. Since the passage of the Affordable Care Act (ACA) in March of 2010 the …
Continue reading “Webinar: Next Generation ACO Model – Overview and LOI Information”
The NextGen ACO: Another Round Opens
by Gregg A. Masters, MPH The Centers for Medicare and Medicaid Innovation has announced the results of its ‘continuous learning‘ commitment model wherein ‘field reports‘ including provider comments and open door inputs are materially incorporated into tweaks of the Medicare Shared Savings Program (MSSP) as risk is progressively adopted by participating ACOs. This ‘new round’ iteration …
Final Medicare Shared Savings Program Rule (CMS-1644-F)
by Gregg A. Masters, MPH Creating consistent high quality original content is hard. At ACO Watch, we’re not in the business of breaking news or high frequency posts to drive eyeballs and traffic to this blog so ‘the numbers’ that might attract advertising or sponsorship (there aren’t any). Instead we (mostly me) watch the developments …
Continue reading “Final Medicare Shared Savings Program Rule (CMS-1644-F)”
The Droids You Are Looking For Are Not Here
by Gregg A. Masters, MPH Beneath the ideological crossfire and mostly bluster of the ACA ‘repeal and replace crowd’, while the latest ‘new, new, thing‘ aka the defacto Rorschach upside of a litany of mostly vaporware or me too ‘meh‘ digital health apps, platforms or S-1 filings (see: ‘Disruptive Idiots from Silicon Valley‘) stumble into maturity amidst …
Continue reading “The Droids You Are Looking For Are Not Here”